As artificial intelligence continues to make remarkable strides, few fields are witnessing its transformative impact as profoundly as medicine. Specifically, robotic systems equipped with AI capabilities are on the brink of revolutionizing surgical procedures, paving the way for safer, more efficient, and potentially autonomous surgeries. Understanding this evolution requires a closer examination of how AI is reshaping surgical practices and what implications it holds for the future of healthcare.
Historically, surgical procedures relied heavily on the manual skills and experience of human surgeons. While these professionals have provided exceptional care, the potential for human error and limitations in precision remains a concern. However, recent advancements in AI technology have introduced new methods of training robotic systems to enhance surgical efficiency and accuracy.
One significant development in this area is the use of deep learning algorithms that allow robotic systems to learn surgical techniques through observation. For instance, by analyzing thousands of recorded surgeries, AI can identify optimal strategies and techniques, effectively ‘learning’ surgical skills. This capability not only helps improve the precision of robotic systems but also equips them with the knowledge needed to perform complex procedures with minimal human intervention.
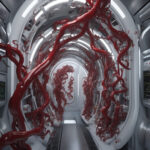
A prime example of this innovation is the work being undertaken at major medical institutions, where robotic systems are being integrated into operating rooms. These robots, supported by AI, can perform specific tasks such as suturing and cutting with remarkable accuracy. This shift marks a notable transition from traditional surgical methods, where the human element was essential, to a model where machines can operate independently under specific conditions.
The advantages of AI-assisted surgeries extend beyond mere efficiency. Studies suggest that procedures performed by surgical robots tend to result in fewer complications and quicker recovery times for patients. For example, a study published in a renowned medical journal found that patients undergoing robotic-assisted surgeries had significantly lower rates of postoperative complications compared to those who had traditional open surgeries. This demonstrates that AI can not only enhance the surgical process but ultimately improve patient outcomes.
Moreover, using AI in surgical settings may lead to better resource management. As robotic systems become more autonomous, they may help alleviate the burden on medical staff, allowing human surgeons to focus on more complex and demanding cases. This collaboration between AI and human professionals presents an ideal scenario where the strengths of both can be maximized for optimal patient care.
However, transitioning to AI-driven autonomous surgeries does not come without challenges. As with any technological advancement in healthcare, ethical considerations arise. Questions regarding accountability in the event of surgical errors, the need for thorough regulatory frameworks, and the implications of depersonalizing medical care are at the forefront of this conversation. Stakeholders, including policymakers, healthcare professionals, and technologists, must collaborate to address these concerns and ensure a smooth integration of AI into surgical environments.
In light of these developments, the role of medical education is evolving as well. Resident surgeons must now become adept not only in traditional surgical techniques but also in operating and collaborating with robotic systems. Medical schools are beginning to incorporate training on AI and robotic surgeries into their curricula, ensuring that the next generation of surgeons is prepared for this swift change in the industry.
In conclusion, the integration of AI into surgical practices promises to redefine the landscape of healthcare significantly. With advancements in robotic systems equipped with sophisticated AI algorithms, we are nearer to achieving the goal of autonomous surgeries. This innovation has the potential to enhance precision, improve patient outcomes, and optimize healthcare resource management. However, realizing this future requires careful consideration of ethical and educational frameworks to ensure that surgical practices remain safe, efficient, and human-centered. The journey toward autonomous surgery is not just about technology; it’s about fostering a healthcare environment where technology complements the irreplaceable value of human care.