Lab-Grown Mini-Brain with Blood Vessels Could Help Slash 90% Neurodrug Failure Rate
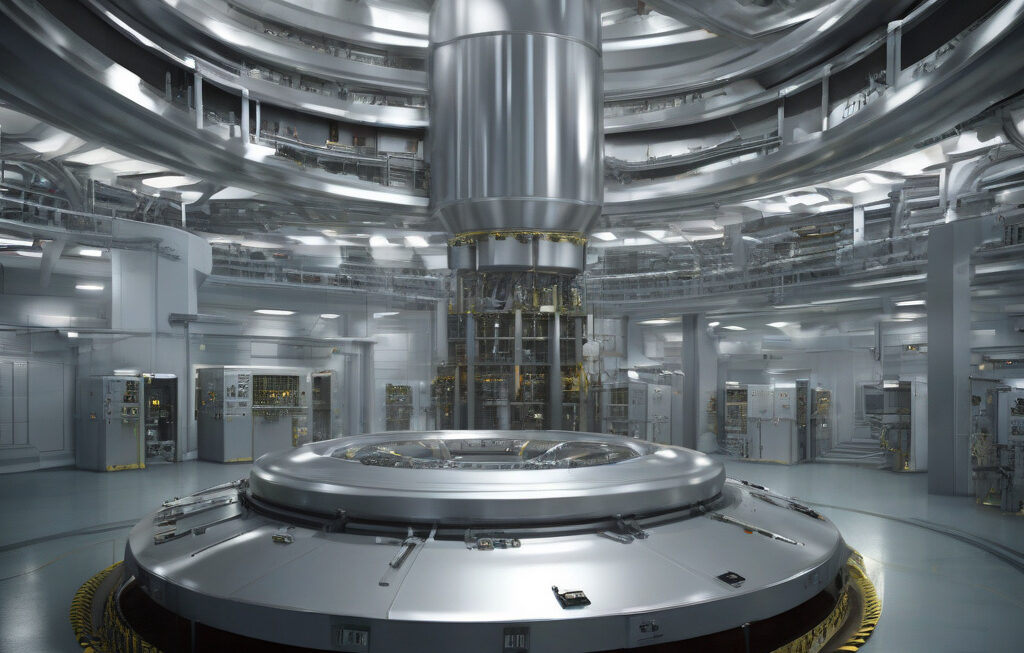
Johns Hopkins University researchers have developed a novel whole-brain organoid. This model is unique because it mimics a real brain’s blood vessels, which are essential for delivering nutrients and drugs to brain cells effectively. The inclusion of blood vessels in this lab-grown mini-brain could revolutionize the way we test neurodrugs and potentially slash the current 90% failure rate in bringing these drugs to market.
Neurological disorders such as Alzheimer’s, Parkinson’s, and epilepsy affect millions of people worldwide, yet developing effective treatments for these conditions has been notoriously challenging. One of the primary reasons for the high failure rate of neurodrugs in clinical trials is the blood-brain barrier, a protective shield that regulates which substances can enter the brain. Many potential drugs that show promise in laboratory settings fail to cross this barrier when tested in humans, leading to costly and disheartening failures.
By incorporating blood vessels into their lab-grown mini-brain model, the researchers at Johns Hopkins University have created a more accurate representation of the human brain’s complexity. This innovation allows scientists to study how drugs interact with the brain’s vascular system, providing crucial insights into whether a drug can effectively reach its target within the brain. As a result, the new organoid model could significantly reduce the number of neurodrugs that fail during clinical trials, saving time, resources, and ultimately, improving patient outcomes.
Furthermore, the lab-grown mini-brain with blood vessels offers a platform for personalized medicine in neurology. Since each person’s blood-brain barrier is slightly different, testing drugs on individualized organoid models could help predict how a specific patient will respond to treatment. This level of precision medicine has the potential to revolutionize neurology by enabling doctors to prescribe medications that are more likely to be effective for each patient’s unique brain physiology.
In addition to its applications in drug development and personalized medicine, this breakthrough in organoid technology underscores the incredible progress being made in the field of regenerative medicine. The ability to grow miniature organs in the lab opens up a world of possibilities for studying diseases, testing treatments, and advancing our understanding of human biology. As researchers continue to refine and improve organoid models, we can expect even more groundbreaking discoveries that will benefit patients and healthcare systems worldwide.
In conclusion, the development of a lab-grown mini-brain with blood vessels represents a significant advancement in neuroscience and drug discovery. By addressing one of the major challenges in bringing neurodrugs to market, this innovative model has the potential to transform the field and improve outcomes for patients with neurological conditions. As we look to the future of medicine, it is clear that organoid technology will play a crucial role in accelerating the development of new treatments and ultimately enhancing the quality of care for those in need.
neuroscience, organoid technology, drug discovery, personalized medicine, regenerative medicine